Alex LaTrenta ‘20, Co-Editor-in-Chief
Despite the chaos of this global pandemic, it is crucial that we remain educated on scientific facts pertaining to COVID-19 in order to best protect ourselves and our loved ones from infection. Below is information from reputable sources such as the CDC, MSNBC, NYC Health, and USA TODAY as of early May which addresses some common inquiries about COVID-19 and how to best remain safe from infection.
Why is the current coronavirus sometimes called COVID-19 and other times SARS-CoV-2?
There are many viral strains within the coronavirus family, some of which are responsible for mild illnesses such as the common cold. The strain of virus currently causing the global pandemic is called SARS-CoV-2 (Severe Acute Respiratory Disease Coronavirus 2). COVID-19 denotes the name of the disease this virus causes in humans (Coronavirus Disease 2019).
If I catch the virus and survive, do I still have the virus in my body after I recover? Am I now immune to SARS-CoV-2 for life?
Once you recover from infection, the virus is eliminated from your body. Your immune system produces antibodies against this specific virus, but it is currently unclear whether those antibodies will protect you from future infection. There have been reports from China of “reinfection” with SARS-CoV-2, but there is speculation that these people may not have cleared the virus from their initial infection which may represent reactivation rather than true reinfection. It is also unclear whether the strength of your immune response—the number of antibodies you produce and their efficacy—might determine if you can be reinfected. If antibodies do make you immune, scientists are unsure whether this antibody immunity will protect you from infection permanently or only temporarily.
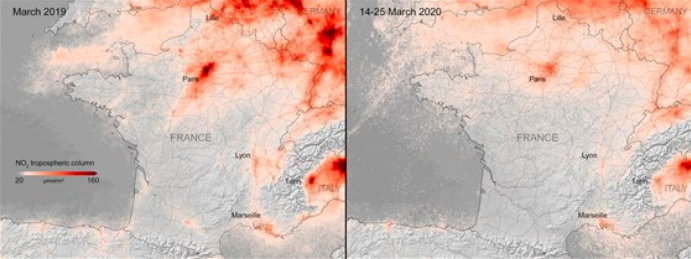
Are there certain environmental conditions (temperature, light) that can destroy the virus, and does that mean that certain climates prevent the spread of the virus?
Although high temperatures and strong UV light can destroy the SARS-CoV-2, there is no evidence that warm weather or sunlight are wholly protective. Countries and states with warm climates still report high infection rates, and thus many scientists believe this pandemic will not be as seasonal as influenza.
Why do young people still need to be concerned about catching coronavirus?
Although the death rate for people under 25 is low, the virus can still cause severe illness in young people, particularly in those with asthma or diabetes. More importantly, older people and people with pre-existing medical conditions are more vulnerable to becoming severely ill and at risk for catching the virus from young people who might be more socially active and mobile. So even if we are not at risk of dying, we need to protect older people in our society—including our parents and grandparents—from infection.
Why do we need to wear surgical or cloth masks in public? Do I need to wash a cloth mask and how/when do I do this? Why do I still need to socially distance when I wear a mask?
Many people can be infected with COVID-19 and show few or no symptoms, but their respiratory droplets are still infectious and can spread several feet just from talking. Sneezing or coughing can create clouds of infectious particles which can travel over 6 feet and hang in the air for hours. Wearing a mask protects those around you from the larger droplets, although it does not stop transmission by the smaller particles. Therefore, masks protect others from your respiratory droplets and can protect you from the larger droplets generated by others. However, only N-95 masks protect from the smaller droplets, which is why we still need to socially distance. Also, wearing a mask reminds us to not touch our face. Besides inhaling droplets, the virus is also transmitted by touching a contaminated surface and then touching our mouth, nose, or eyes. Since viruses can live four to seven days on metal and plastic, up to 4 days on glass and paper, and up to 24 hours on cardboard, it is important to disinfect our hands when we come into contact with potentially infected surfaces and to train ourselves to not touch our face. Cloth masks should be washed every day with the hottest water possible and laundry detergent.
How is COVID-19 different from having the flu? Don’t people get hospitalized and die during flu season?
In the 2018 to 2019 flu season, according to the CDC, approximately 35.5 million people got the flu, 490,600 were hospitalized (1.4%) and 34,200 died (0.1%). In the two months since cases have been diagnosed in the US, 1,079,943 people have tested positive for SARS-CoV-2 and 63,615 have died (6%). COVID-19 has a 20% hospitalization rate and approximately 10 to 25% of those patients eventually need intensive care. Most of those in the ICU must be put on a mechanical ventilator to help them breathe, and even then 50 to 80% of those patients die. The mortality rate of COVID-19 varies depending on the country but is approximately 2% in China, 7% in Italy, and 7 to 10% in New York City. In summary, only 1.4% of people with flu are hospitalized versus 20% with COVID-19 and only 0.1% of flu infections result in death versus 7 to 10% for COVID-19 (if we exclude the questionable data from China). Of course the total number of people infected may be higher with COVID-19 due to undertesting and asymptomatic infections, but COVID-19 clearly causes more severe illness than influenza with higher rates of hospitalization and death. Due to the high hospitalization rate and requirement for ICU care, COVID-19 can easily cause health care systems to become overwhelmed by the volume of beds and intensity of medical expertise required to care for these patients. SARS-CoV-2 also seems to be more infectious than influenza.
Why are COVID-19 infections so severe relative to the common flu?
The flu mostly infects the upper respiratory tract cells, such as the nose and mouth, while the SARS-CoV-2 virus primarily affects cells in the lungs. SARS-CoV-2 also appears to travel through the body and can affect white blood cells, the kidney, liver, heart, and brain. Through an unknown mechanism, it also causes the formation of blood clots throughout the body which can cause stroke and fatal blood clots to the lungs. Many flu deaths are because of secondary bacterial infections or because the virus makes pre-existing health conditions such as lung or heart disease worse. SARS-CoV-2 kills people more directly because of its effects on multiple organ systems and blood clotting. Mortality is also higher because SARS-CoV-2 can cause an exaggerated immune response (so-called “cytokine storm”) which causes a flood of inflammatory cells into the lungs which then fill up with fluid, which limits oxygen exchange.